CRAFTING WELLNESS STORY
"Cancer May Have Started The Fight But We Will Finish It."-Oncology Nurse
We sat down with Oncology Nurse Em to talk about her life as a nurse in such an emotionally charged and difficult speciality. Change the way you look at things and the things you look at change. Emily says, "I absolutely love what I do, you know, for all the reasons that people say oncology, nursing is hard are the very reasons I absolutely love it. My preceptor when I started, told me, 'You know, death for these patients is a total release of suffering. Cancer is one of those diseases that causes unimaginable suffering and a peaceful passing is a blessing.' So, ever since she told me that it kind of changed my perspective."
TRANSCRIPT
Brooke Smith
Welcome to MDF instruments Crafting Wellness Podcast. I'm so excited today to introduce you to Emily. She is a travel Nurse in Oncology.
Emily
My name is Emily, I go by @thatspitfirenurse on Instagram. I am an oncology nurse. I do outpatient clinic nursing. And I've been an Oncology nurse about four years now,
Brooke Smith
A pretty serious nursing specialty. Can you tell us a little bit about what drew you into oncology nursing specifically, and why you chose nursing and why you're a nurse and just how you kind of just came to this career path?
Emily
Yeah, of course. So I kind of took the long way around to get to nursing. I did nursing as a second career. So originally, I went to, I did undergrad, and I was gonna go to med school, so did all the classes for med school. And then I worked in emergency room. And I did not like the way doctors treated patients. So I ended up talking to my dad who asked me like, do you really want to go to med school? Like, can you give me a good reason I couldn't and he always kind of pushed me towards the nursing route. So I decided that you know, after working towards for most like I will I want to be a nurse and honestly I feel like it's the heavens like opened up like it was a great decision for me. And I did do a BSN program in North Carolina. And also ironically enough, I was like I can't do oncology. oncology is too hard. You know, I don't have the heart for it. So my program was about four semesters. And the first semester I was like, I want to do oncology and I want to do nursing administration. Like, that's where I see myself. And then as as I went through my program, you know, I realized I really liked talking to patients and you know, learning their stories and I was like, You know what, let me challenge myself and pick oncology. Alright, Capstone, I kind of had a choice between oncology nursing, that was my top choice. And then my second choice was like the cardiothoracic ICU. So very different spectrum. Um, but honestly, I got oncology, and I loved it. I think, you know, it does take a special person to be oncology nurse, I think it's, you know, it's more of a calling, then I feel like other specialties maybe pediatrics, but it I don't know, like, I fell in love with it. When when I when I started there as a student on my floor, I really like I don't, I always had an interest in palliative care as well. And oncology and palliative care go hand in hand. So I really liked you know, being able to, you know, see patients at end of life, because that's kind of where my heart lies. I want to do I really like palliative care, hospice, end of life. And it's, it's funny, like, I can't see myself doing anything else. Like, I absolutely love what I do, you know, for all the reasons that people say oncology, nursing is hard. Other reasons, I absolutely love it. You know, it's very, my preceptor when I started, told me, she was like, you know, death for these patients is a total release of suffering. You know, cancer is one of those diseases that causes in unimaginable suffering. And for them, you know, passing a peaceful passing is a blessing. So, ever since, you know, she told me that it kind of changed my perspective. And, you know, now, like, I've seen myself going into palliative care as an oncology, like nurse practitioner, and you know, helping patients decide, you know, helping them pass peacefully, you know, and pass where they want to pass. So, kind of a long winded answer, but yeah, like oncology nursing is definitely it's a special type of nursing, but it's so I think it's so underappreciated. And it's amazing.
Brooke Smith
Yeah, I imagine that it's not the easiest of specialties, just because I know that you probably have harder days than, you know, like a different kind of specialty in nursing, where it feels like they could probably go through several shifts and not have, you know, a death. I imagine for you, it's a more common thing in your life. Would you say that's true?
Emily
You know, I think so. And I think it's, it's different now that I've shifted into the outpatient setting, you know, in the, inpatient oncology, at least in like a medical oncology, you know, you see a lot of symptom management, you see patients at their worst, you know, they're only admitted if they, you know, if we can't, if they can't manage their symptoms, outpatient. So being outpatient has been very, you know, very different, you know, we still we see patients from time of diagnosis all the way to either, you know, survivorship or unfortunately like hospice, but outpatient has been awesome because there's a lot more, you know, you see a lot more positive stories, you know, people like you know, being able to ring the bell when their cancer treatments over you know, and like graduating and going from, you know, being cancer fighter to a cancer survivor. That's, you know, that helps balance out because you see a lot more of those cases outpatient than you do on The opposite. So it's been it's been.
Brooke Smith
That's awesome. So for everybody who doesn't know who's listening or like me, can you explain the difference between outpatient and inpatient? And how that changes? Depending on does that change where you work then? Are you still like, Are there outpatient in the hospital still? Is that how it works?
Emily
Yeah, so, inpatient is like traditional bedside nursing. So usually like 12 hour shifts, you know, what you typically think of as like, you know, being a bedside nurse. Outpatient, you do have a lot of different options. I work in a clinic. So I see patients one on one with a provider, you know, we see patients in clinic, you know, I handle phone calls, all that jazz. And then there's also outpatient infusion, which is kind of like a, you know, an intermediate between bedside nursing, outpatient, you know, clinic nursing, because you're still doing a bunch of skills, you're you're you're administering chemotherapy, a bunch of, you know, like electrolytes, blood, blood products, and whatnot. But you're not, you know, you're working different hours working outpatient hours. So 410, four times by dates, the lifestyle I think, you know, if you're kind of moving towards like, I don't know, like retirement revenue, like a lot, you see a lot of older nurses in the outpatient setting, because it's, you know, it's a better lifestyle. You know, you if you're working, you don't work nights, you don't work weekends, you know, you don't work holidays. So it's a very different lifestyle, it's very different type of nursing, you know, it's not, you don't do a lot of nursing, like skills, per se, unless you're working infusion. But for me, I like it, because I'd like talking to patients, that's my opinion, or saying very good, like people
Brooke Smith
personally, you know, when we're in the hospital, or we need it, we need care, you know, we're scared and feel alone and afraid. And like, all those things, so having someone that like, can calm us down or relate to us or make us feel like it's going to be okay, I mean, I think that's the most important thing. And that's why I love nurses. That's why I have like, such an affinity for you guys. Because I think it does take a really special person kind of person to get into nursing, and you guys are really empathetic, you have big hearts, you want to be there for people during the most vulnerable times. And I think it just it takes a really special really special soul it's really not an easy thing and er setting you could have a nurse like okay, they're having to work weekends or they're having to work holidays and that kind of thing and maybe in an outpatient situation not doing that but you're dealing with you have other issues and stressors that you're dealing with that kind of got will compensate for the maybe the schedule that's a little more normal stress level, I imagine and just the things that you have to go through and see and witness and help with as that kind of nurse like I'm sure can be daunting so I wonder for you if but we're always talking about mental health because like I said, you know, you guys are it takes certain kind of person to get into health care. So naturally the medic generous all that it's an easier position for people to take advantage of you because you're in a position of service. And in that kind of way, you know, people get there on medication they can they're not themselves all the time. And I know that especially in health care can take some some abuse both by patients and also by staff and all that. So it just kind of wonder how you manage just the stress of your your career and able to like stay so positive, and keep going through all those hard days.
Emily
Yeah, I mean, so for me, I am very good at compartmentalizing. So, you know, when I when I go to work, I'm there, you know, I'm very present. Like, I always say that the moment I swipe in is the moment I'm 100% like 110% present for my patients, you know, I will give, you know, give myself freely. But the moment I swipe out if meantime, you know, I 100% leave work at work. And I'm fortunate to be in a career, I can do that. Even if I have you know, like tougher patients, which you know, or sad or cases that while on, you know, I give myself some time to reflect. And usually it's on the car ride home. And then when I get home when I walk into my door, I don't think about it. When I've done that pretty much for the past four years, and it's really helped because, you know, we do see, you know, a lot, you know, we you are participating in other people's lives, you know, and you see them, especially with oncology, you know, you see the worst, you know, people out there worse, you know, Uncle cancer is one of those diagnoses that, you know, is life changing. And I've seen even like the, you know, the most stoic, like strong men crumble down, you know, so, I definitely leaving work at work was very important to me, and then you know, the time I'm home, you know, my my best friend, my roommate is also a nurse and you know, we were able to converse, you know, and kind of share stories if we want to, but if you know if not, we usually just hate you know, we'll hang out we'll walk dogs. We don't do anything healthcare related. Um, and also like You know, we do deal with quite a bit at, you know, at, at the job, you know, with abuse and whatnot, but for me, unless a patient physically attends that's different, but, you know, if they're frustrated, I get it, you know, at the end of the day, I get to walk, you know, I gotta go home, I don't have cancer, you know, I'm very fortunate. And so I can empathize with these patients from like, no one. And most of the time, you know, they'll apologize, like, I'm so sorry. And I'm like, It's okay. Like, you know, I get it, like, it's, it's, it's a terrifying diagnosis. And that fear of the unknown can change can change people, and can make them act out in ways that's not that's not normal for them. And, typically, you know, you give them time to vent, you give them time to, you know, give them their space, and they'll come back, and they'll apologize, but for me yet, being empathetic, putting, you know, putting myself in their shoes is really helpful. And I don't know, like, ever since COVID, like, I've been probably, like, started doing these tiktoks just to like, distract people. You know, there was, again, a lot of fear of unknown among staff. And I think that kind of just, like, evolved, and now like, you know, I do a lot of posts about, like, you know, just being a be, you know, enjoying yourself, you know, nursing is one of those careers, that it's so difficult. So you have to, you know, you have to make time for yourself, and you have to enjoy, you know, make fun of yourself, you know what I'm saying? And I'm a terrible dancer, you know, those tick tock videos, I was like, I'm terrible. But if I can make someone laugh, you know, that's the best thing for me. So even if I even at my own expense, that's totally fine.
Brooke Smith
Spoken like a true nurse. No. It's funny, though, because obviously, we find the trend really is as they always have a creative outlet. Whether it's, you know, social media and finding tiktoks, or blogging, or writing or dancing, or singing or acting, or whatever it is, there's always a creative outlet. Because I do really think that there is something to that, where it's like, you have this creativity in you as well, that needs to come out. And it's such a great healthy way to express it. Because, you know, for me, like music really helps me process like my emotions. And when I'm going through something, I find songs that I can really relate to. And it helps me kind of like process. And I love what you're talking about where you're saying, you know, sometimes I need the car ride home, to process the day. And I think that's really smart, you're like, but once I get home, and I walk in that door, like I leave work, where we're where work is, and I'll pick it back up the next time I'm there. And I think that's a really brilliant way because what a great way to kind of decompress. I don't know how long of a drive you have. But I can feel that because in the car and stuff sometimes for me, when I go through something like the car right back or whatever, I just maybe need 15 minutes to just process and then I level myself out and be like, Okay, I gotta move on. And gratitude is something Another thing you're touching on, which I think is so important to just remember how good we have it. And you know, you're talking about like why at the end of the day, I don't have cancer and I get to walk home, I get to go home and be healthy. And like I'm not, I'm not in that position. And I think it's a really great way to kind of bring yourself back to gratitude. But I still feel like, I can relate because my dad right now he's he's fighting cancer, and he's actually in the hospital. And he's not it's really rough. But like the last two days, he's been hallucinating. And he's doing crazy things that like my dad would never do. And I guess like last night, in the middle of the night, he thought he was in war. And so he thought he had been shot. And so he's like hallucinating and like yelling at the healthcare people and like, I don't even know, just being physically he's old, you know, older, but just still being physical. And I'm like, wow, my dad is like the most docile. Personally, he would never, like be irate to people or like it's not like him at all. But like you were saying, you know, when you have cancer and you're fighting for your life, and you have all these medications you're on and things interact with other things that people are taking. They're not themselves, but at the same time, I still really feel like nurses and healthcare workers in general, like you guys do get a lot of, of that energy. That's hard, you know, because it's like, it's not it's not personal, though. And it sounds like that, you know that at the end of the day, it's not personal. It's not actually them attacking you, verbally or whatever it is. It's just, they're sick and they're fighting and they're, they're, you know, trauma does a lot for two people, it changes them and they cannot act like themselves. But I just think it's important to kind of touch base on the fact that like it's excusable In one in one way, it's like, I can understand why it's happening. But at the same time, it's just not okay. Like, I feel like for you guys especially like, I get why it happens, but it's just, it's hard for me to swallow it because I'm like, Well, yeah, but it's not an it's an excuse, but it's really not. Okay. And like, I just hear a lot about a lot of nurses getting, you know, sometimes, like, they get accidentally hit maybe, or maybe on purpose or, you know, just all kinds of crazy things happen to you guys. And it's just like, I don't know, I mean, I don't really know what can be done to protect you guys better, but I just, you know, especially with what you're doing, it's just like, it's a real thing that nurses go through that is just not, you know, not good.
Emily
Yeah. I mean, it's tough, right? Because it's, you know, a lot of times these patients are confused, you know, and being in a hospital, you know, does not do anything for their confusion. You know, I've been choked. I've been punched, you know, you know, it's a potential the job, I don't think it's part of the job, right. But I think I take more issue with like, the verbal abuse. Because, you know, unless a patient is like, blatantly confused, you know, I've had family members cuss at me, you know, like, denigrate me, and there's no reason for that, you know, I always say, like, if I were on the street, right, if we were not in the hospital, I wasn't wearing my scrubs, would you talk to me the same way that you're talking to me right now? Right, I feel like, you know, there's, there's a fine line between you're advocating for your family member, if you're, you know, if you're they're advocating for yourself, versus just being overly rude. And, you know, we're, I always say, like, I work for the hospital, I don't work for you, right, I'm here to help you, I'm not here to serve you. And I think a lot of you know, these, these hospitals now are so focused on customer or patient satisfaction scores, you know, that they're there, they're less concerned about their staff, you know, staff satisfaction, right? Because, I think, yes, sort of, like Medicare and Medicaid, you know, it's all, it's all about money, you know, ultimately, the end of the day. So, it's a shame, you know, it's like, there have been so many bills, you know, put forward, you know, to protect health care workers, you know, health care workers have died, you know, we've been seriously injured, have died. On the job, especially my, you know, my colleagues in the ER, you know, they really get the brunt of it, both physically and verbally. And, you know, it's unacceptable with mental health issues, being on the rise, you know, keep it some people can't, you know, they can't, they can't help it, right, their mental illness is, is a killer, especially untreated mental illness. And, you know, we, as much as we want to help these patients, you know, we weren't, you know, we can't, you know, we can't monitor them all the time. You know, we can't force them to go to rehab, we can't do anything. No, we can, you know, we can lead a horse to water, but we can't make them drink. So I think there's, there's, this is a very multifactorial issue, that I think, you know, we're, a lot of healthcare workers are speaking up, you know, about, and I think, you know, people have to take a notice. So, because people won't tolerate anymore, you know, I think COVID really was like, straw that broke the camel's back, you know, health care workers were literally, you know, putting their lives on the line for their patients and hospital ministration, like, you know, didn't do anything to reward them, you know, or to, like, you know, to me, we were called healthcare heroes, but, you know, we were treated like zeros, you know, so, there's a fine line, like, you know, I obviously, I want the best for my patients, and I, you know, I want I want them to be safe, and they want them to, you know, to get better. But I also am, you know, I am not willing to tolerate the abuse that comes with it, and I'm not sure if there is a good answer, you know, my, I'm just glad there's a lot of talk about it right now. And, you know, it's, it's a hot button issue. So,
Brooke Smith
yeah, I think like, it's important to talk about because we don't talk about it, we can't change it, we can't fix it and can't help it. But I just think people need to understand and know that it's happening because I think what happens is there's there's maybe some protection there of maybe the patient more than the staff excute making excuses justifying it, you know, all of these things. It's like, Oh, it's okay, just move on. I want to talk about let's just get to the next thing. But the problem with that is that when we don't talk about it, then we can't people don't realize how common it is. And and then you think you're the only one you're like, Oh, I'm probably he that's probably you know, just happened to me this week. But it's it's fine. Let's move on. But really, it's it's a lot more common than I think people even realize because once they start talking to each other, it's like, oh, well, yeah, that happened to me yesterday, too. And this is, you know, and this kind of behavior, because there needs to be protections put in place or um, Have some kind of way to help advocate and protect the health care worker, because at the end of the day, like, you're there to help, but you're not there to like take abuse and be treated, mistreated. And it's like, there is a fine line between understanding like, okay, someone's mentally ill or they're not themselves right now they're on heavy medication, you know, there are these conditions that make you understand logically what's going on. But at the same time, would they be talking to the doctor like that? It's a respect issue. And I think if the the staff or the hospital or places not requiring people to be respectful, then you're just kind of leaving it up to them to have to decide when they're going to be respectful or not. So it's just too good to talk about because it's not okay. And it's not fair, especially in the specialty that you're in. I know, just from hearing what my dad was doing and mortified because I know that that's not who he is. But at the same time, I'm not there, but they don't know Him. And you know, and this is the, this is what's happening and I bet for healthcare workers out of this not okay. So much excuse you can make them. It does take compartmentalizing what you're talking about, about just being able to compartmentalize, okay, this is this is how the day starts, this is how the day ends, like now I'm going to take time for myself. Can you walk us through a little bit? I know you did a little social media post on it. But can you walk us through a typical day for you? And are you working Monday through Friday is more stable hours? Can you tell us a little bit about what what an oncology nurse day like is for you and outpatient anesthesia? Sure.
Emily
Um, so my hours are eight to 430, I work five eighths, I've also worked for 10s, which I prefer. But yeah, so pretty much my job entails. So I, if I'm seeing patients, so we'll have clinic days, and then we'll also have like admin days, during the clinic day, which are the majority of the days, we will see patients from eight to like three, and then No, so it's usually the team is a nurse, the provider, like a doctor, and then we have a mid level. So either a PA or an NP. And you saw at my current facility, we see all the patients first so the nurse goes in, you know, talks to the patient, we do you know, we have a questionnaire, we just make sure they're doing okay, ask them usually how they're tolerating their chemotherapy or radiation. If there's any concerning issues, and then we bring it, we go back, talk to them, talk to the doctors, and then they go in to see the patient. And that kind of goes, you know, throughout the day. And we do that just so you know, the doctor can, you know, focus on really what matters, you know, what the patient, you know, how they're doing, versus having, you know, them having to ask all the different questions. And then when we're not seeing patients, you know, we get a lot of phone calls and a lot of symptom cars, you know, there's a lot of symptoms with chemotherapy and radiation, and we encourage our patients to call because, you know, sometimes these symptoms can be, you know, either a sign of potential allergic reaction or, you know, something that, you know, if it's so on totally intolerable, it means that we may have to change the dosage. So it's your phone calls, answer messages, and then, you know, if I have downtime like this, this clinic is awesome. All the nurses and the providers are in this one, like a one big floor. So it's cool, I can chat with the other teams, you know, and, you know, just hanging out. So there is not a lot of downtime, but there is no just just enough to to get to know it, everyone who's working there. So that's good.
Brooke Smith
So I have a question about oncology nursing, for us specifically, just trying to understand it, do you treat them like all different kinds of cancers? Are there certain cancers that are coming to this outpatient facility where you're doing this,
Emily
but I'm working actually in a supportive care department. So like palliative care, and, you know, we see patients of, you know, every different type of cancer, but the clinic, you know, I work on a metal floor, so Medical and Surgical Oncology. So we see solid tumors, there's, there's another floor, these are the radiation oncology patients and then another for that years with blood base cancers. So you know, we see everything I've rotated through, you know, quite a few specialties which I, which I really enjoy doing, because like I said, I'll see every, you know, every type of cancer patient in my particular department, these doctors, you know, the providers that we're working with are top of the game, you know, this is the number one cancer hospital in the world. So, you know, these doctors are awesome. And they're, it's a great, you know, they're they're always willing to teach and the nurses, they're, you know, also top notch. So, it's cool, it's a great learning environment. You know, I'm kind of nerdy like that I like to know, like, you know, everything about these handlers, so it's fun to ask and, you know, they're obviously very passionate about it. So So they'll talk, you know, they'll talk your ear off. And I love
Brooke Smith
that. Yeah, they imagine with your specialty, you're also getting to know your patients pretty well, right? Because I think typically like if you're an ER nursing or something like that, like a patient comes, they might stay in hospital for like a week or something, and then they're gone. But with what you're dealing with, I imagine it's more several week process radiation,
Emily
generally the process, we see them as a new patient, you know, they established care with us. And then, you know, we so we deal with the chemotherapy, like radiation is another, you know, is a whole nother area of oncology nursing, which is exceptionally fascinating, but I actually just starting to learn about but yeah, we see them, you know, every, depending on what their cycle chemotherapy, you know, how often they're getting it, we'll see them, you know, every two, three weeks, maybe even every month, just to check in, make sure they're doing okay. And then, you know, when they finish treatment, you know, depending on you know, what, what our scan, so make sure they're doing okay. And then as you know, if they're, if their cancer is responding and doing well then you know, we kind of increase that interval which we see them up for the first like for the from title diagnosis, we see them pretty much like two or three times a month.
Brooke Smith
Yeah, wow. That says it's gotta be rewarding to to just see like, the star of the journey of like, okay, I have cancer, and how are we going to navigate this to the end of like, the ringing the bell to like, Okay, I'm a cancer survivor now, and like, hopefully, it will go into remission. And just like, seeing the whole process of the start to the finish has got to be really rewarding.
Emily
And it's very, you know, super emotional, obviously, like, you know, I've worked in both, like, I've worked in a breast oncology clinic, and, you know, these, most of the time these cancers were caught pretty early, you know, so, but it's an emotional time, you know, like, no one wants to be told they have cancer, you know, no one wants to be told they have stage four cancer, you know. So it is emotional. And it's also emotional, like, towards the end, you know, either you know, as, as they graduate, or, you know, them being told, I'm sorry, like, reach the, you know, the limit of the treatment options that we have. So, it, it is a very emotional journey. And, you know, like I said, you know, even the, you know, the most stoic stubborn patients, you know, they will feel they'll break down eventually. So, it's interesting to see, you know, how they know, their journeys, and their course and know, in clinic, we see patients, you know, throughout their cancer journey. So, you know, you get to know them pretty well, you know, you get to know like, oh, they come in, you're like, they don't look so good. Like, they're all acting themselves, or, wow, you know, you look great, like, no, and you see, the patients that lost their hair, through their treatment, come back, and then you know, their hairs going back and you're like, wow, like, you know, it's like, you look like a different person. So it's, it's cool.
Brooke Smith
If you could go back and tell your younger self, some piece of advice, what would it be? Do you have anything like inspiring that you could that or something you wish you had known? That, you know, now, anything like that, I think,
Emily
you know, as corny as it is, like, you know, to not be afraid to kind of break out your shell, you know, I used to be this very introverted, very shy individual. And now, you know, I'm a completely different person. And I think, you know, nursing was kind of something that I come from, if I'm going to do this, ended up loving it, you know, oncology, I was like, I don't know, if I have the heart for doing this. Love, you know, I love it. And then, you know, being able to travel nurse, you know, kind of helped me really break out of my shell, like socially. I'm very, like, I'm super extroverted now, but I used to be like, really not. So definitely just like, continued like, you know, don't don't be afraid to step out of your comfort zone, because honestly, it's done nothing but wonders for me.
Brooke Smith
Are you still travel nursing now? Or are you more settled in Texas? Because I know you were doing travel nursing. Can you talk a little bit about that?
Emily
Yeah, so I did travel nursing for a year. It's actually what I found outpatient nursing. I did six months in New York City and then six months at a small clinic in Winston Salem, North Carolina. Um, and I really enjoyed it. I just got fed up with agencies. You know, it's they're very shady and I did not like that. You know, so I was like, I knew as an oncology nurse MD Anderson is number one and I was like, I would love to work here. So I applied for this for a staff job and honestly, it's I'm so happy like I'm so happy I love Houston. I love being here and love MD Anderson. And yeah, it's weird going back from like, you know, being a staff nurse but I think being a travel nurse and having you know, being exposed to so many different things and you know, being put in like any scenario and having to adapt quickly is really helped me here. You know, they can put me pretty much anywhere and I'm like, what do you need me to do? So that's that's helped in your I'm very grateful for my travel experience,
Brooke Smith
I think like what you're talking about is really great. It's great advice. It's almost like studying abroad kinda when you're in college, I feel like everybody should maybe go travel nurse for just a year just to see what it's like go somewhere new step into different roles because you really have to be on your feet. It's funny that you're talking about the whole agency thing, because I just did a podcast with travelers about that. And it's pretty crazy to think about what the hospitals are billing and then the agencies taking money, but not telling you how much they take, like, in just as the fight for that like is it sounds very shady, and like another thing that we need to change as far as moving forward with transparency and fees and things like that? Totally. Yeah. So what do you do for fun? Have you found some interesting things in the US tend to do? Yeah, have you been able to kind of, like, translate that into us in this new place that you're living? I used to be that dog. So what do you like to do for fun?
Emily
Oh, I, one of the reasons I went to travel nursing is because I like to go out to eat, explore new restaurants and bars. And you know, Houston is a great foodie city. So many restaurants, so many bars. So I've been enjoying going out, you know, on the weekends with with my roommate and meeting new people, obviously, like walking the dog. The dogs love it here too. So it's, yeah, just trying new restaurants every weekend. That's why I've been such a foodie
Brooke Smith
tale. I absolutely love food I love like, I'm on Yelp. I'm on Google, I'm trying to figure out okay, like what's really good to eat. I'm all about trying new things. But like finding the homemade version, or this like yummy new drinks or spots. So I totally feel you on that. And there's a lot of great food, while I get Mexican food to feel like
Emily
Oh, definitely.
Brooke Smith
Who inspires you in your life who is you kind of like look up to and kind of want to emulate
Emily
there are two people, they're both very, very close to me, my mom, and actually my best friend. And all the enough, their personalities are pretty much the same. I think that's why I'm so close to my best friend. But my mom, my mom is the most patient person that I know. You know, she kind of taught me to be, you know, to be very respectful. Same thing with my dad, but she's also you know, taught me a lot about empathy. Which, obviously, you know, that's most important part of my job. It's really why I'm good at my job. So I'm definitely grateful for her. She's also you know, super selfless and caring. And then my best friend, Emily, who, you know, has, she's been, you know, she's in my Instagram as well. But she is probably the best nurse that I know. She's a pediatric oncology nurse, but she is if you like an angel on Earth, just a very selfless sweet, just like kind hearted person. I actually hated her when we first met her because she was so nice that I thought she was like, so fake, I kind of realized, Oh, she's she is a very sweet person. You know, she really, she's, she's very bubbly and outgoing. I think she kind of helped, you know, bring that out me. She's the other half of my, my tattoo. You know, we're we're ying and yang, you know, opposites but very much, you know, complement each other perfectly. And she, you know, she inspires me to be better nurse every day, you know, for patients love her. She's a pediatric oncology nurse. Like, you know, I've always had respect for pediatric nurses anyway, but pediatric oncology takes a very special person and she loves her job. She's very, very, very good at it. You know, she kind of put herself out there and she's been excelling. And you know, it's great to see her every day, you know, do what she does, and do what she loves and enjoy it. So
Brooke Smith
I love that so much. So how did you guys meet? Did you meet in school or tell the story of how you guys met each other?
Emily
So we actually met on our first our first job. So we had both graduated from nursing school and started listening for together and I started about a month earlier than she did. But then you know, we kind of grew we did a lot of orientation together and then you know, we we became really close friends we started hanging out and then now like pretty much inseparable. I call her like my life wife. You know, she's here in Houston with me obviously, you know, I live I've been living with her for the past year and a half or so. But ya know, it was like it we hit it off and like yeah, literally, like, stuck together since.
Brooke Smith
I love that so much. And it's it's really important to have, I think in anything that you do in life just to have friends, someone that you can trust and turn to and confide in and the fact that You're both in nursing and you're both in oncology what the difference being adults versus pediatric is just gotta be such a nice like common baseline to but you can understand each other understand the kind of days you're having be there for each other and then also know when like to be quiet. Also know when like, Okay, I don't want to go there today, but I think it's so special to have that support and I'm so glad that you have that. You know, we can get her on the podcast too. And then we should do like a double podcast and have the two besties on getting Yang and oncology nursing and actually sounds amazing so I mean,
Emily
I actually gifted her a pediatric MDF Stethoscope so
Brooke Smith
good. Yeah, we're gonna have to get her involved. Now we can just think like, what you guys do is so important and so special and appreciate you guys both so much for what you're doing out there in the world, just making it a better place and bringing health to people and hope and patience and kindness and love and all the things that our world needs more of. So thank you so much for doing what you do.
Emily
I love it and I wouldn't do anything else.
Brooke Smith
I know you're on Instagram I imagine tick tock with the dance moves you're talking about. Go ahead and drop your social handle for anybody who wants to come take out take a watch of the GED take a dance lesson from you or I should pass all this stuff on like what the day in life is like she's constantly giving knowledge advice, everything on her social media. So
Emily
So yeah, my Instagram is that Spitfire nurse EM. which is definitely a accurate description of me. And then my Tiktok handle is m Jamie E M. J A Why Am I
Brooke Smith
perfect? Yeah, I was gonna ask why do you call yourself a Spitfire nurse, that Spitfire nurse How did that little nickname come to be? So I
Emily
used to be like, very soft spoken and not kind of like, you know, I would never stick up for myself and then became a nurse. And I've been told I've gotten in trouble for yelling at people, particularly residents, you know, just for all in like, you know, to defend my patient, you know, I never speak up unless a I know I'm right. And be you know, it's to defend, you know, to protect my patient. And you know, the times I have spoken up, yes. Like, could I have done a little better nuanced way? Yes. But then the day, you know, like I did what was right by my patient, so I don't regret it.
Brooke Smith
See, there's the empathy of that again, though, because it comes from like, you're sticking up for other people. You know what I'm saying? Like you haven't said like, oh, when it comes to my patients like protective, like, I'm coming in there, and I'm going to say something and it's like, but we need to also learn how to because I'm the same way. If someone is like, hurting a friend, family member, like I get really protective, but sometimes I have a hard time doing that for myself. So it's really great to think about like, love yourself, like you love when people you know and defend yourself stick up for yourself to like, it's good, because it's, I think about that sometimes I'm like, when I let you know someone do that to my mom or my dog or whatever it is. And I'm like, no, like, I'm not them. Don't do that, sweetie, you know, like, I gotta love myself, like I love other people, and has
Emily
great money because like no one wants to be yelled like, no doctor wants to be yelled at by like a tiny Asian girl, like in the hallway. I'm like, come on, like, let's talk about this. They're like, Oh my God, and my charger is just like
Brooke Smith
you come from like thinking that that's where you were going to go originally, like going back to what you were saying earlier about how you thought you wanted to be doctor and the med school route and all of that. So I think you kind of it's funny because I talked to people who who a lot of people thought that they were going to go in and maybe become a doctor or something like that. And then they realized the nursing was for them. And vice versa. Sometimes when and thinking about religion nursing and decided I actually want to do the doctor thing. It's just very interesting roles, how one really speaks to you over the other. You know, what I also love about nursing that we didn't really cover too much was just the fact that there's so many avenues and so many things you can do different specialties ways to like keep advancing your education if you want to like it's just it's endless. It's absolutely endless with all of the knowledge that you accumulate and then that knowledge you can keep and use just for any other position that you're doing. Do you have any I know oncology's for you. That's where you're you're at the do you kind of see yourself extending education or anything down the line. Are you pretty much like this is this is wearing set?
Emily
Well no, I definitely. I have been putting off going back to I love school like I've been putting off going to grad school just because it takes I changed my mind quite a bit and it took me a really it took me about four years to figure out what I really want to do and what I really enjoy doing. But you know, I definitely I'm going to apply get my doctorate and then doing a dual fellowship in both oncology and palliative care. Because palliative care is a very big specialty. But I want to stick solely with cancer patients.
Brooke Smith
Yeah. So can you explain what that specialty is? For anybody who doesn't know?
Emily
Yes. So palliative care is a, it's kind of a broader term, it pretty much focuses on symptom management, quality over quantity. But, you know, a lot of people interchange palliative care and hospice, which is not accurate. You know, palliative care is an umbrella term and includes hospice, but hospice is very specific, you know, in order to qualify for hospice, a patient has to be, you know, have a terminal illness of six months of life expectancy or less, but palliative care, anyone with a complex disease can can qualify for palliative services. So it's a huge, you know, range of diseases, cancers, obviously, one of them. But, you know, it's, it's one of those services we do, you know, we do a lot of symptom management, you know, we, besides just doing medication, and we can connect patients with like integrative medicine, you know, to do alternative medicines, you know, alternative therapies, for patients who may be a little bit more, you know, tired of just medicating and medicating, you know, we have other options for them, you know, we deal with, you know, we help patients with spiritual issues, you know, emotional, psychological, you know, it's, it's a very umbrella term, you know, pretty much our job is to make sure that, you know, we're maximizing their quality of life, you know, the, the medical team focuses on the quantity, but we focus a lot on quality and making sure that they have everything, they need all the resources, they need, all the resources the caregiver needs, to, you know, make, make sure the patient is comfortable. Yeah, sounds like you're focusing
Brooke Smith
on like, the whole entire person, not just the not just the disease, or the thing you're trying to fix, but also like, the mental struggle with it, and the maybe like, nutritional symptoms of it, and like, all the whole, just the whole package of all of the things that can go wrong, and that we need help with when we're going through something so stressful. Our bodies, I love that I didn't even know that was a thing, but it's, that's really great to know.
Emily
Yeah, I mean, it's, um, it's definitely an underutilized specialty. I think, you know, part of my goal with, you know, my social media account is to, you know, make people more aware of what palliative care is, and to kind of dispel the rumors that palliative care, you know, is only hospice. You know, there's a lot of education that needs to be done. Because I think, you know, we can't even say pilot carrying on without patients, you know, becoming anxious, you know, they think that okay, like palliative care means I'm dying, like, no, like, hospice, yes, but like palliative care, you know, we're here to help you cope, you know, we're not here to, you know, be like, everything's done. Like, no, no, and I think, you know, in hospitals, they cancel palliative care inappropriately all the time, you know, they only console and life which, you know, there needs to be work there too. But yeah, I think as nurses, you know, it's really important for us to kind of, you know, explain you know, the difference to patients because, you know, at the end of the day, you know, we want to see the patient succeed as well. You know, we have to deal with the brunt of the symptoms and you know, a lot of the emotional aspects of palliative care can be very beneficial for them.
Brooke Smith
Well, thank you so much for sharing that Emily thank you so much for joining our MDM interamente crafting wellness podcast it's been such a pleasure and we're gonna have to I think we're gonna have to do another one with your best friend who's also named Emily I'm so awesome Emily nurses Wilson Oh, oncology one adult one pediatric I think we need to do it. Yin and Yang duo
Emily
are totally
Brooke Smith
we'll have some more fun but it was such a pleasure having you on and I'm really excited to see all the great things you're gonna do and follow your journey even more on social.
Emily
Thank you so much for having me. I really you know, I enjoyed talking with you and yeah, it's it's been a pleasure.
WELCOME TO THE NEW SCHOOL.
LET'S ROLL
BE THE CAUSE
This is our oath and we need you. The WORLD needs you. We need your heart, your mind, your skills, and your partnership
MORE CRAFTING WELLNESS STORIES
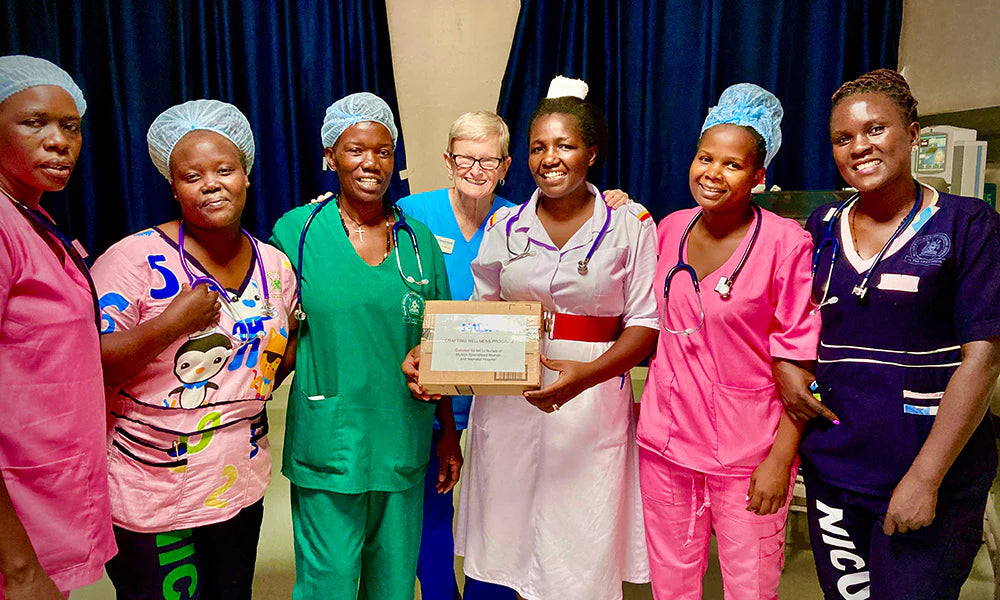
IN HONOR OF OUR WELLNESS HEROES
Health Volunteers Overseas
At MDF Instruments, our commitment extends beyond crafting superior medical tools; it encompasses a vision for a healthier, more equitable world. We are honored to partner with Health Volunteers Overseas (HVO), an organization dedicated to… More
Read moreUniCare Specialized Polyclinic
Through the best clinic services they can provide, UniCare Specialized Polyclinic is a dream-team of passionate clinicians dedicated to improving community health and wellbeing. This is why MDF is honored to be partners with UniCare, providing them with stethoscopes and blood pressure monitors.
Read moreEmpowering Healthcare Access
At St. George's International Medical School, students are more than just learners; they are agents of change. Through the Global Medical Brigades, an initiative aligned with Global Brigades, they transcend classrooms to touch lives in
Read more